Floaters Surgery
What are floaters?
Floaters are shapes that people can see drifting across their vision. Floaters are small bits of debris floating in the vitreous jelly inside the eye. They can come in a variety of forms such as hair-like, small black dots, short squiggly lines, small fly-like or tadpoles, or even large cobweb shapes. Shortsighted people tend to suffer from them more, and they increase as we get older.
What causes Floaters?
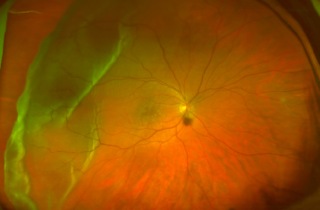
The eye is filled with a clear jelly-like substance called vitreous. The vitreous sits behind the pupil and lens. The jelly is made mainly of water with a meshwork holding it together, and forms 80% of the eyeball volume. As we get older, a process known as vitreous syneresis occurs; the meshwork breaks down and lakes form. The solid portion of the gel forms debris. The debris casts shadows onto the retina, which we see as floaters.
As the vitreous gel separates, it peels away from the retina and this can cause people to see intermittent flashes of light. The flashing light will usually subside over 4 to 12 weeks, but in some patients it may take a little longer. When a posterior vitreous detachment occurs people often become aware of a cobweb or net curtain-like floater that can be quite intrusive at first. A PVD can develop earlier in life if you have undergone a cataract surgery operation.
What complications could occur?
In the vast majority of cases floaters are harmless and represent the normal, natural (although occasionally annoying) ageing change of the eye. They usually become much less obvious with time as the brain adjusts to the change and eventually filters them out.
Very rarely during the development of a posterior vitreous detachment, the vitreous gel can be stuck to a patch of retina and cause a retinal tear. A retina tear can occur in up to 10% of PVD patients. If the seal of the retina against the back of the eye is broken, fluid can start to track in behind the retina causing it to detach from the back of the eye a little like wallpaper peeling of a wall. A retinal detachment is an uncommon event that occurs in approximately 1 in 10,000 of the population in general. Usually, if a tear develops in the retina people experience a very marked shower of floaters associated with flashes of light in their peripheral vision. The light is usually persistent and occurs in daylight. Some people notice a curtain effect coming in from their peripheral visual field. This requires urgent attention by an eye doctor.
In a different situation, the vitreous detachment can pull on a retinal blood vessel, and if the blood vessel is broken then the vitreous jelly fills with blood, and this is called a vitreous haemorrhage. A small shower of spots in your vision suggests a mild amount of blood in the vitreous. If you see large dark blobs in your vision or if your vision is generally very hazy or blurred, then this suggests a much larger haemorrhage in the vitreous jelly.
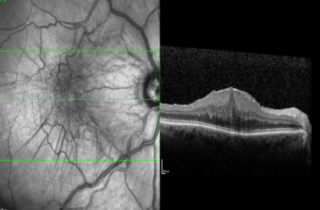
What assessments do I need?
If you have new symptoms of a PVD (floaters, flashes, shower of spots) it is important to have a prompt and thorough examination of the retina to search for any retinal breaks. If a retinal break can be discovered before a retinal detachment develops it can be treated with the laser to seal the break and prevent a retinal detachment. Finding a retinal break can be difficult and requires a very complete examination of the edge of the retina.
The pupil must be dilated for a proper exam, which includes indirect ophthalmoscopy with scleral depression. This is the exam where the retina specialist wears a light source on his head and examines the retina with a handheld lens while pressing gently in on the edge of the eyeball with a blunt, smooth-tipped instrument (scleral depressor) to bring the periphery of the retina into view. Examination with a special contact lens for viewing the retinal periphery may also be performed to be sure if any and all retinal breaks are located.
Treatment options
Since floaters do not harm the eye, and in the vast majority of people, they do not cause a significant problem, and no treatment is generally recommended for them. This is because your brain constantly adapts to changes in your vision, and learns to ignore floaters so that they do not affect your vision.
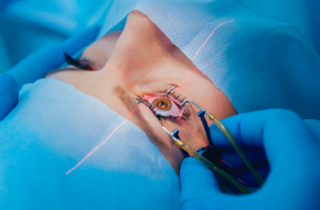
In people with very severe floaters or in those who cannot adapt to them, the floaters can cause visual disturbances that affect their quality of vision. The persistent floaters can interfere with social, work and driving life. It is possible to carry out an operation to the eye to remove the vitreous gel (vitrectomy), which will also remove the floaters. A complete consultation is recommended with your retina surgeon, and you can be counselled about whether this operation is suitable for you. The “Floaters Only Vitrectomy” operation offers an excellent outcome in the vast majority of patients.
What are the risks of surgery?
Vitrectomy floaterectomy surgery carries with it the risk of various complications. The most common side effect of vitrectomy surgery is the development of cataract at an earlier stage than it would have done otherwise. Rarely this can be immediately after the surgery but more commonly; this may come on 2-3 years after the operation.
The most severe complication from this kind of surgery is blindness in the eye, usually because of a severe bleed during surgery or an infection in the eye after the operation. This is an extremely rare occurrence (approximately 1 in every 2000 cases) but it is important that patients are aware that there is a chance that it could happen, albeit very small and a rare occurrence.
There is a less than 1% risk of patients developing a retinal detachment after the surgery which can sometimes lead to reduced vision in the eye afterwards. Once again this complication is unlikely to happen after surgery. In this situation, further surgery is required to reattach the retina and Mr Muqit is a retinal surgeon who can manage this complication.
What anaesthetic is required for vitrectomy surgery?
Vitrectomy surgery can be performed under local anaesthetic or general anaesthetic. Under local anaesthetic you will be awake but you will not feel any discomfort as the eye will be numbed with an injection. You will not see the operation and the other eye will be covered. Local anaesthesia can be given with sedation that will help you to relax during surgery if you are feeling anxious about the operation. If a general anaesthetic is chosen then you will be fully asleep. The decision as to which type of anaesthesia is most suitable will be made following a discussion between you and your surgeon.
What should I expect after the Surgery?
Although vitrectomy surgery is a major surgery, it is rarely very painful. It is normal to experience some discomfort in the eye after surgery but this usually relieved with simple painkillers such as paracetamol or ibuprofen.
The white of the eye will look red and the eyelid may appear swollen following surgery. You may also experience some watering from the operated eye and a gritty sensation during the first month following surgery as any stitches gradually dissolve. The redness, eyelid swelling and watering will gradually improve.
Vision in the operated eye will usually be very blurred for the first few weeks but will slowly improve. The final visual result may take several weeks and you may require new glasses. The floaters disappear in almost 99% of patients.
Will I need to instil eye drops after the Surgery?
You will be given an eye drop to reduce inflammation (steroid drop), another to prevent infection (antibiotic), and sometimes additional drops to keep the pressure inside the eye within normal limits. You will be advised on how many times a day to use the drops before you leave hospital. Use the drops regularly until your first postoperative outpatient visit. You will then be given further instructions on how long the drops need to continue for.
What can I do after surgery?
If you have been given any posturing instructions then these should be followed. You can bath or shower, but avoid splashing water near the eye. Generally you may do anything with which you are comfortable. Most people choose not to drive over the first few weeks.
If a gas bubble is used for surgery,
You must not fly until the gas bubble has gone and you must inform the anaesthetist if you require a general anaesthetic for any operation while there is gas in your eye.
How much time off work will I need?
Most people will need at least two weeks off work after surgery. Sometimes this may be longer. While there is gas in the eye the vision is quite poor and the ability to judge distance is affected. The amount of time off work will depend on the kind of work you do and the kind of surgery that is done. This will need to be discussed with your surgeon.
Scientific Evidence
The advice in this booklet is based on a variety of sources, including latest research published in peer-reviewed scientific journals. Please ask your surgeon Mr Mahi Muqit if you require further information about this.
To book an appointment call +44 7717 203564 or email pp@retinasurgeon.uk.com
Treatments & Surgery

Hole
A small, circular gap opens up at the centre of the retina. Causes blurred vision and distorted vision, and patches of missing vision at the centre.

Disease
You must be screened for diabetic retinopathy, as you may not notice changes to your vision. Diabetes damages small blood vessels of the retina, leading to bleeding in the retina and fluid leakage at macula.
Detachment
The retina is the light sensitive film at the back of the eye and retinal detachment is an emer gency wher e the retina peels away to cause a shadow or loss of vision.

Floaters are shapes that people can see drifting across their vision. Floaters are small bits of debris floating in the vitreous jelly inside the eye.
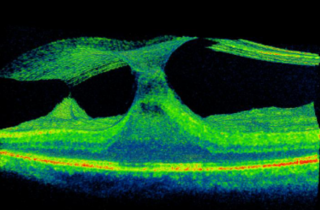
Traction
The vitreous gel shrinks and pulls away from the macula, but the vitreous remains partially stuck and pulls on the macula surface to cause mechanical traction
Surgery
Mahi Muqit performs routine and complex cataract surgery for all types of cataract and vitreoretinal patients, and has expertise in lens implant exchange surgery.
Membrane
Scartissues forms over the Macula, it contracts, crumples, and squashes the Macula resulting in distorted and/or blurred vision.

Surgery
Mahi Muqit performs a wide range of surgical procedures, and offers a comprehensive vitreoretinal surgery service.



