Vitreomacular Traction Surgery
What is vitreomacular traction?
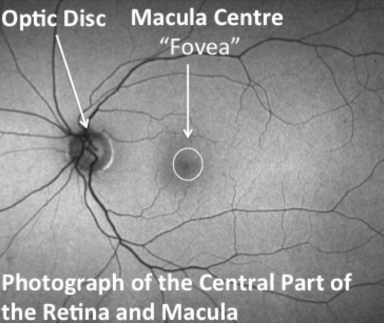
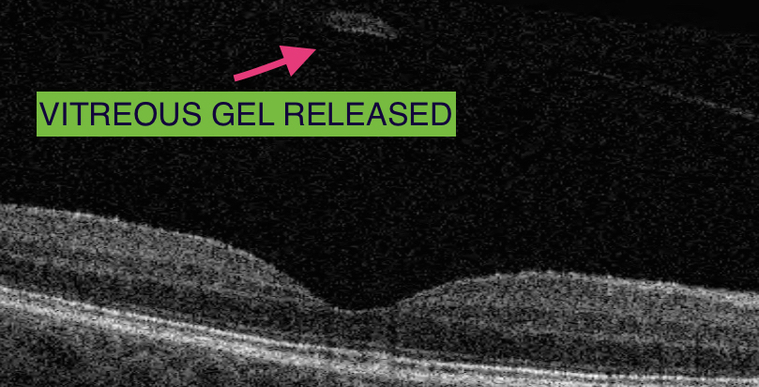
As we grow older, the vitreous gel that fills the eye shrinks and pulls away from the macula. The macula is made of special nerve cells and it provides our sharp central vision needed for seeing fine detail (reading and driving etc.). Sometimes as the vitreous pulls away from the macula, it remains partially stuck and pulls on the surface.
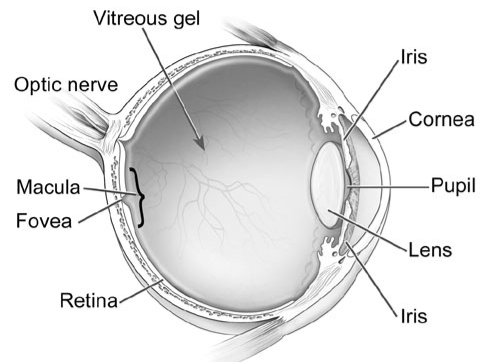
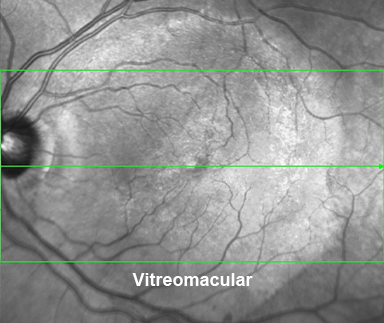
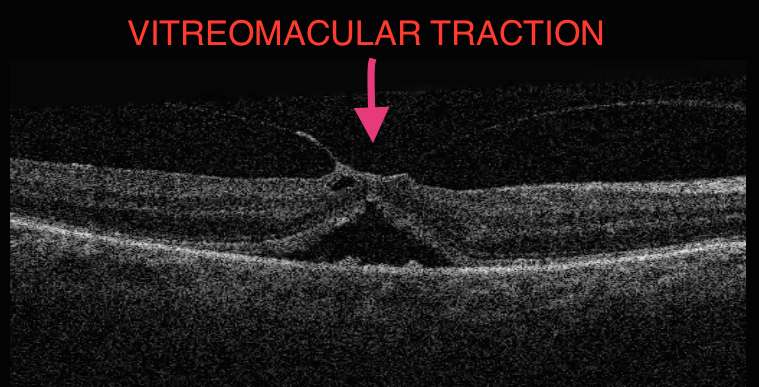
This pulling and distortion of the normal macular structure is called vitreomacular traction (VMT), and this can result in distorted and/or blurred vision.
Why do I have vitreomacular traction?
The vitreous gel shrinks and pulls away from the macula at different rates in each person, but it occurs in everyone with time. VMT only occurs when there is an abnormally tight adhesion between the shrinking gel and the macula.
The VMT may affect the other eye, and is common in people with macular degeneration and diabetic eye disease in later years.
Assessment for vitreomacular traction?
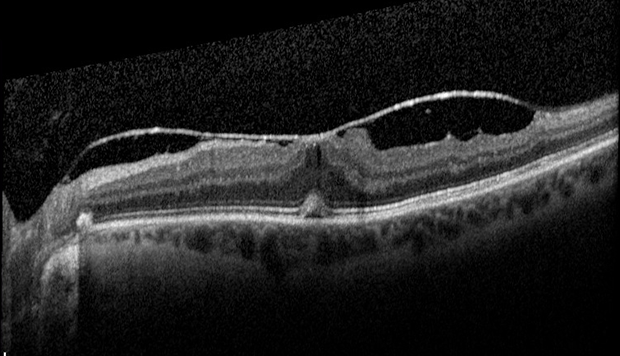
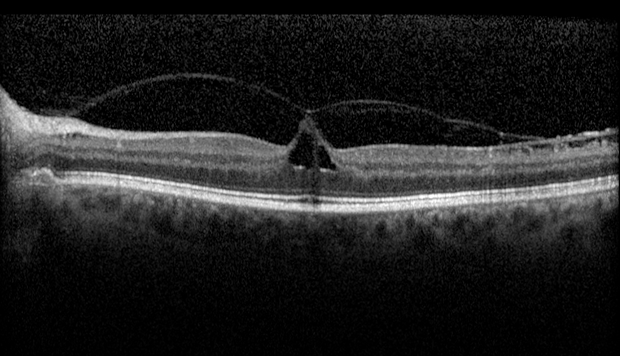
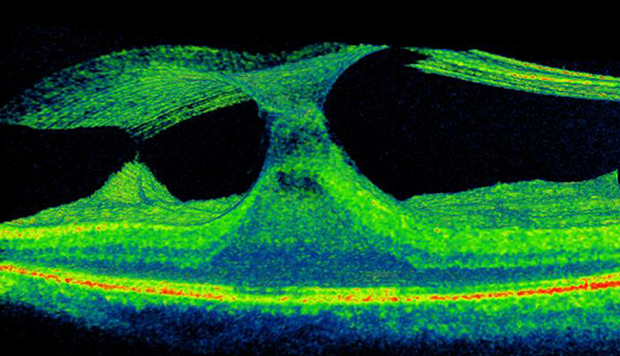
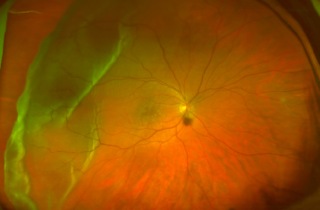
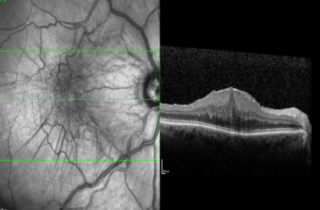
A careful retinal examination can reveal signs of VMT, including distortion and elevation of the retina, and fluid accumulation within areas of stretched retina. Your eye doctor is able to detect vitreomacular traction during an eye examination following the use of eye drops that temporarily make your pupils large. A special photographic scan of the back of the eye can confirm the presence of a vitreomacular traction and assess how mild or severe the condition is.
Your retina specialist Mahi Muqit will assess your symptoms to help you decide whether to proceed with surgery.
What should I expect with a diagnosis of Vitreomacular Traction?
In many cases, the discovery of vitreomacular traction is by chance at a routine examination and the vision may not be affected. The vitreomacular traction tends not to change and does not always affect vision. The VMT may cause no symptoms at all in its mildest forms. Sometimes, VMT worsens and the increased traction results in blurred or distorted central vision. Treatment for vitreomacular traction is only required in those cases where the vision has been affected.
Vitreomacular Traction Treatment & Surgery
In cases of VMT where the vision is unaffected, no treatment may be necessary. Follow up examinations are necessary in certain patients to monitor for worsening of the condition. Your retina surgeon can discuss the natural history with you in detail, and provide advice and reassurance where this condition has been detected without any symptoms.
Sometimes as the vitreous gel continues to shrink, its adhesion to the macula will release and the VMT will resolve without treatment (in 10% of patients). In a small number of patients, the vitreomacular traction may produce a small macular hole. The management of the particular macular hole needs to be discussed with your retina surgeon.
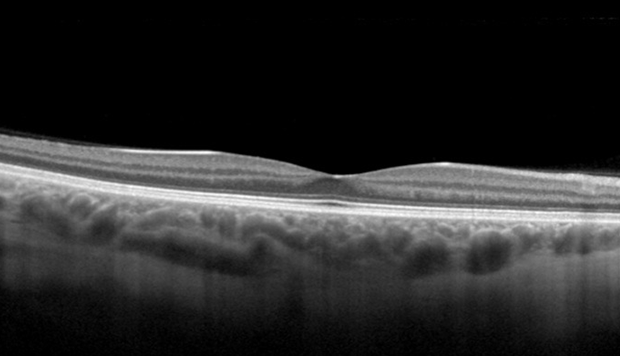
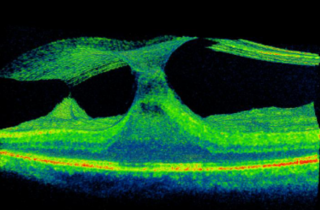
The 3D Optical coherence tomography scan shown below, this demonstrates the key problems. The vitreous becomes like a “cone” and the epicentre is located directly at the centre of macula, known as”the fovea.” If this condition does not spontaneously recover to normal, the vitreous can either be separated from the fovea using an injection of Jetrea or by vitrectomy surgery.
Injection Treatment
A new drug called Ocriplasmin (“Jetrea”) has recently been approved by the National Institute for Health and Care Excellence (NICE) in the UK for patients with vitreomacular traction with severe symptoms, or VMT and a macular hole with symptoms. The drug is injected into the vitreous through a self-sealing microincision in the wall of the eye (“intravitreal injection”). You will need to discuss this treatment option with your retina surgeon Mr Mahi Muqit before making an informed decision about whether an injection is a suitable option for your VMT condition.
“Jetrea is approved by NICE (UK)”
Vitreomacular Traction Surgery
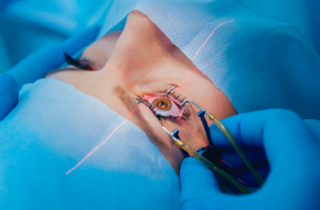
Vitrectomy surgery can be performed under local anaesthetic or general anaesthetic, and does not usually take longer than an hour. It can be performed using a local anaesthetic injection with the patient remaining comfortable and awake during the procedure. It is very important for the patient to stay still, especially during the very delicate manoeuvres when the vitreomacular traction is removed from the centre of the macula. The vitreous is replaced by natural aqueous fluid produced inside the eye. In some cases, the surgeon has to leave a special gas bubble inside the eye which disappears on its own after a few weeks.
Following treatment of vitreomacular traction, the vision is typically more blurred and it can take months for it to improve. The Surgery is usually successful in reducing the distortion in vision due to the vitreomacular traction. If the vision had not been distorted prior to vitreomacular traction release, improvement in the sharpness of vision and reading is less predictable.
Risks of Surgery for Vitreomacular Traction Release
What should I do following surgery?
Following surgery, you will be given eye drops to use for a few weeks, which will help the eye settle from surgery. The operation does not require staying in hospital longer than one night and patients are typically reviewed in clinic a couple of weeks after surgery. In some occasions, you may be asked to position your head in a certain way for some part of the day for a number of days. Otherwise, you can do most daily activities although you should abstain from unhygienic environments and anything that puts the eye at risk of injury.
How much time off work will I need?
Most people will need at least two weeks off work after surgery. The amount of time off work will depend on the kind of work you do and the kind of surgery that is done. This will need to be discussed with your surgeon.
Scientific Evidence
The advice in this booklet is based on a variety of sources, including latest research published in peer-reviewed scientific journals. If you require further information about this, please ask your retina surgeon Mahi Muqit.
To book an appointment call +44 7717 203564 or email pp@retinasurgeon.uk.com
Treatments & Surgery

Hole
A small, circular gap opens up at the centre of the retina. Causes blurred vision and distorted vision, and patches of missing vision at the centre.

Disease
You must be screened for diabetic retinopathy, as you may not notice changes to your vision. Diabetes damages small blood vessels of the retina, leading to bleeding in the retina and fluid leakage at macula.
Detachment
The retina is the light sensitive film at the back of the eye and retinal detachment is an emer gency wher e the retina peels away to cause a shadow or loss of vision.

Floaters are shapes that people can see drifting across their vision. Floaters are small bits of debris floating in the vitreous jelly inside the eye.
Traction
The vitreous gel shrinks and pulls away from the macula, but the vitreous remains partially stuck and pulls on the macula surface to cause mechanical traction
Surgery
Mahi Muqit performs routine and complex cataract surgery for all types of cataract and vitreoretinal patients, and has expertise in lens implant exchange surgery.
Membrane
Scartissues forms over the Macula, it contracts, crumples, and squashes the Macula resulting in distorted and/or blurred vision.

Surgery
Mahi Muqit performs a wide range of surgical procedures, and offers a comprehensive vitreoretinal surgery service.



